Can routine clinically used scan protocols performed on CTDI test objects predict patient dose?
November 21, 2019
Presented at the annual meeting of the European Congress of Radiology (ECR) in 2018.
PARTICIPANTS:
An Dedulle, MSc Leuven, Belgium
Disclosure: PhD Researcher, Qaelum NV
Niki Fitousi Leuven, Belgium
Disclosure: Research Director, Qaelum NV
Jurgen Jacobs, MSc Leuven, Belgium
Disclosure: Co-founder and CEO, Qaelum NV
Hilde Bosmans, PhD Leuven, Belgium
Disclosure: Co-founder, Qaelum NV Research Grant, Siemens AG
Aims and objectives
In this study it is evaluated whether dose estimates from phantom data are representative for patient dose data and/or whether phantom acquisitions could therefore act as a surrogate for patient dosimetry surveys. This study was performed for Computed Tomography (CT) examinations of the skull, chest and abdomen.
The study was triggered by the current practice and the legislation to come in the EC Member States. The European Basic Safety Standards (BSS) define Diagnostic Reference Levels (DRLs) as dose levels in medical exposures, for typical examinations for groups of standard-sized patients or standard phantoms, for broadly defined types of equipment [1]. The core idea is that standard-size patient data or standard phantoms could be used to determine the DRLs. Regardless of the methodology adopted by the competent authorities, the major aim of DRLs is to detect malpractice, such as medical devices with a mean dose level that is unexpectedly high in comparison to the DRL, and initiate optimization. This study aims to verify whether indeed phantom data measured during routine quality assurance (QA) can predict standard-sized patient doses.
Methods and materials
Phantom data: Phantom data for present study were collected during routine annual quality assurance (QA) testing of the CT scanners by the medical physicists in radiology. Following the Belgian protocol for these annual tests [2], the dosimetric output in terms of CTDIvol for protocols of routine CT skull, chest and abdomen exams has to be registered. The protocol stipulates that comparing scanner specific data to the data of a group of other scanners may trigger immediate action already during the annual test (when radiographers/radiologists are around) making the annual test more clinically relevant. This test was included in our protocol and applied on 16 scanners in radiology departments of our Quality Control (QC) network.
For this purpose a homogeneous cylindrical polymethyl methacrylate (PMMA) phantom with a diameter of 16cm is used for the skull protocol and a cylinder with a diameter of 32cm is used for the chest and abdomen protocols. After a scout view, all preprogrammed exams of the list are planned on this phantom scout view. The scanner then indicates the CTDIvol that would be used by the CT scanner for this particular scan. This estimated CTDIvol is registered for this study and represents the mean dose level of a CT exposure for a standard phantom. During routine QA, in other tests, the accuracy of the CTDIvol indication is verified with the same phantoms, using a pencil type ionization chamber with a sensitive length of 10 cm (RTI Electronics).
Patient data: The collection of the patient data in the university hospital of Leuven is performed with the dose monitoring system (DOSE by Qaelum) that is installed in the hospital. The dose monitoring system collects all patient dose data and automatically generates summary reports that are required annually by the regulatory agency (FANC in Belgium). These reports are configured to include data of three months for a maximum of 100 exams for each report for the skull, chest and abdomen protocols. The mean dose from groups of standard-sized patients, in terms of CTDIvol for skull, thorax and abdomen (single acquisition), was retrieved from these reports for each protocol and each CT scanner in the study. Patient dose data of other hospitals were also processed following the guidelines of the FANC.
In a retrospective analysis the correlation between phantom dose and patient dose data for the year 2016 was evaluated for 16 CT scanners, including different models from various vendors (Siemens, GE, Toshiba and Philips). A statistical program (GraphPad Prism, GraphPad Software Inc. USA) was used to analyze the data. D'Agostino & Pearson omnibus normality test was applied to the data. Pearson correlation between the phantom and patient CTDIvol data was calculated and the significance was evaluated with two-tailed p-values with a confidence interval of 95% (p < 0.05).
Results
1. The data passed the D'Agostino & Pearson omnibus normality test (p > 0.05) for all three scan protocols: skull, chest and abdomen.
2. For the skull protocol, data was collected from 15 scanners. There was a weak Pearson correlation between phantom data and patient data of 0.55, but nevertheless it was significant (p = 0.035). The analysis showed 2 outliers (build-in ROUT method with Q=1.0%) [3]; when these points are excluded the Pearson correlation is improved to 0.92 (Fig. 1).
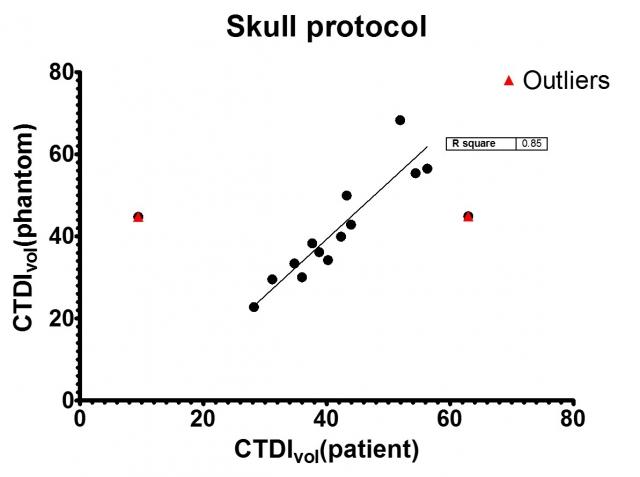
Fig. 1: The CTDIvol from phantom data as a function of the CTDIvol from patient data for the skull protocol.
References: Department of Radiology, University Hospitals of Leuven
3. For the chest protocol, 12 data points were analyzed (Fig. 2). The correlation was not significant (p = 0.098).

Fig. 2: The CTDIvol from phantom data as a function of the CTDIvol from patient data for the chest protocol.
References: Department of Radiology, University Hospitals of Leuven
4. For the abdomen protocol, 13 data points were analyzed (Fig. 3). The correlation was not significant (p = 0.991).

Fig. 3: The CTDIvol from phantom data as a function of the CTDIvol from patient data for the abdomen protocol.
References: Department of Radiology, University Hospitals of Leuven
Conclusion
Only for the skull protocol, phantom tests could predict scanner behavior for patients. For the chest and abdomen protocol, the phantom tests could neither predict mean patient dose for the CT scanners nor the fact whether they were outliers. This may be due to (1) unrealistic tube current modulation (TCM) behavior on the CTDI phantoms, or, (2) with the 32cm phantom representing already an overweight patient, we enter a range in which the scanners apply a proprietary approach that is different from the majority of the patient cases, or (3) an unrealistic estimated CTDI value is displayed after the scout, in part inaccurate without actually running the exam. In earlier phases of our project, it had been verified whether this practice would be acceptable, but there was no thorough study done. There are obvious limitations to the phantom that we use. The phantom is only a homogeneous cylindrical phantom and, apart from x-ray attenuation, it is not representative for a human body. Most skull protocols however do not use tube current modulation (TCM) so patient doses are more easily predicted with the phantom. For the chest and abdomen protocols, an anthropomorphic phantom could be used. An evaluation of TCM behavior on anthropomorphic phantoms compared to patients should be performed first. In our hospital we only have an anthropomorphic chest phantom (lungman, Kyoto Kagaku, Japan). We have carefully validated this phantom for chest x-ray applications and the phantom seems promising for dosimetric applications of chest imaging indeed [4]. We expect that the indicated CTDIvol from a standard chest CT planned on that phantom would correlate better with the patient dose data. A disadvantage of the anthropomorphic phantom is that it can only be used for on-site scanners. However, our medical physics team is also engaged in other centers. It would be difficult to carry several anthropomorphic phantoms to other centers.
Our analysis showed that evaluation of dose with simple homogeneous, cylindrical phantoms cannot replace a patient dose survey. The use of specific anthropomorphic phantoms instead of the current homogeneous, cylindrical phantoms might improve the estimation of TCM behavior on phantoms compared to patients. However anthropomorphic phantoms are expensive and difficult to carry along. Evaluation of mean patient dose of a CT scanner by means of a patient dose survey is indispensable. A platform for patient dose monitoring can improve access to patient data for the medical physicist and it allows access to patient data remotely and 24h/24h.
References
1. Basic Safety Standards directive - 2013/59/EURATOM. Official Journal of the European Union, 2013.
2. Belgian Hospital Physicist Association – Belgisch protocol voor jaarlijkse kwaliteitscontrole van X-stralenapparatuur: de CT scanner. BHPA, 2014.
3. Motulsky HM and Brown RE. Detecting outliers when fitting data with nonlinear regression – a new method based on robust nonlinear regression and the false discovery rate. BMC Bioinformatics, 2006.
4. Rodríguez Pérez S, Marshall NW, Struelens L and Bosmans H. Validation study of the thorax phantom Lungman for optimization purposes. Proc. SPIE, 2017.




